Travel vaccinations are big business, with some costing hundreds of pounds to administer. Visit somewhere tropical and you could be spending thousands on you and your family. With Brexit around the corner, we may be swapping short haul flights for longer ones – so what can practices do to capitalise on this and offer more vaccinations to patients – and is it worth it? Practice Business gets a shot in the arm
In 2017 the average UK resident spent 10.2 days abroad. In total, we made a total of 72.8 million trips outside the UK – a trend that shows no sign of slowing down, even with the looming spectre of our exit from the EU. The most popular destination for sun-seeking Brits in 2017 was Spain, with 15.8 million visits, but there are increasing numbers of holidaymakers and travellers exploring the globe – and exposing themselves to potential healthcare risks.
In the UK the NHS routine immunisation (vaccination) programme should ensure that people born here are protected from some of the world’s most common – and previously deadly – diseases. The success of this programme is one of the reasons why the NHS is the envy of the world; it’s also why, when we travel to developed countries in places like the US and Europe with similar vaccination programmes in place, we don’t need any vaccinations or protection.
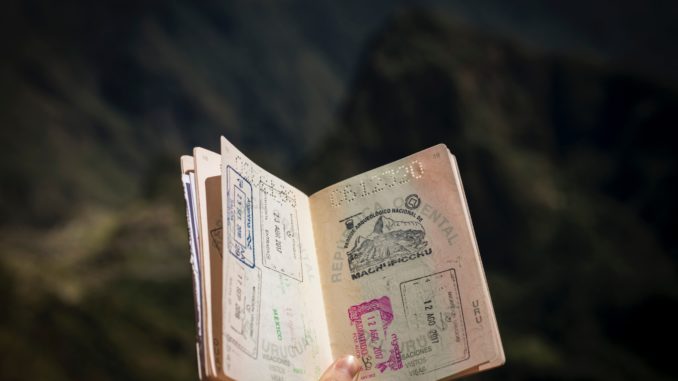
Patients travelling to developing nations across the world may be exposed to diseases that the NHS doesn’t routinely vaccinate against, including yellow fever, typhoid and hepatitis A. Some vaccinations are so important that they must be documented, including the International Certificate of Vaccination or Prophylaxis (ICVP) which much be shown before you enter or leave certain countries.
If patients are uncertain about what vaccinations they need to travel, they should be encouraged to visit a website called Travel Health Pro which has information on the vaccines that globe-trotters might need if they’re visiting any of the 238 destinations on its list.
What vaccines are funded by the NHS?
The Green Book contains all information on the vaccines provides by the NHS, including remuneration for each. Practices need to sign up to the additional services for providing travel vaccinations in order to be able to offer these services and be paid for them. Travel vaccinations which are currently funded by the NHS include:
- hepatitis A vaccine (monovalent vaccine)
- combined hepatitis A and typhoid vaccine
- typhoid vaccine
- combined tetanus, diphtheria and polio vaccine
- cholera vaccine
For all other vaccines, patients will need to arrange and pay for them themselves.
How much will they pay?
The BMJ refuses to provide fees for vaccinations, suggesting instead that practices charge a fee based on the costs of the vaccine and the medical time.
To get an idea of costs, a leading high-street pharmacy currently offering vaccination programmes charges £165 for a course of Rabipur Rabies, £135 for a course of HBvaxPRO and £75 for a single Viatim Hepatyrix injection.
Is it worth offering travel vaccination services?
Offering travel vaccinations can be profitable for a practice, says Jane Greenfield in Guidelines for Nurses, but she suggests practices take a cautious approach as there are risks and costs to consider. Before offering travel vaccinations, all surgery staff should have an ‘understanding of the complexity of travel health to ensure safe and best practice,’ she writes.
Travel vaccines are NOT provided through ImmForm, which means that your practice will need to register with an online ordering system provided by pharmaceutical companies to access travel drugs; you will also need somewhere to safely and securely store them.
The decision on whether to offer travel vaccinations through your practice will be influenced by factors, including the likely local demand, expected revenue, the population and the local competition. Practices should consider how many requests they are likely to receive for travel vaccinations and weigh this against the bureaucratic burden of ordering, managing and administering vaccines. In areas where there are already established providers – GP surgeries and/or pharmacies – practices should also consider whether the effort in promoting travel vaccinations will generate a significant return on investment.
Setting up a travel clinic
In urban areas, with a high potential population of travellers, practices may consider setting up a dedicated travel clinic to remove the burden from working GPs. Such clinics can benefit patients by providing them with a comprehensive and dedicated service, says Jenny Greenfield – and practices can benefit by freeing-up consultation time as the number of general appointments taken by patients with travel-related queries decreases.
In a detailed analysis of the benefits and challenges of setting up a travel clinic she suggests that practices ask themselves four questions before setting up a travel vaccination clinic.
- How much will it cost to set up and run a clinic? Potential costs include staff, occupying the clinic or treatment room, office supplies and the purchase and maintenance of equipment.
- Is the expense of setting up the travel clinic justified by the number of potential patients? This could be assessed by auditing the number of patients asking for travel advice in the last 6 months
- Is an appropriate space available that can accommodate a vaccine fridge, couch and resuscitation equipment?
- Are any of the practice staff already trained in giving travel advice and immunisations? Do the staff have access to up-to-date information?
The decision on whether to offer travel vaccinations is one that should be made based on sound fundamentals, around the capacity and capability within the practice and the likely demand from the local population.
Don’t forget to follow us on Twitter, or connect with us on LinkedIn!

Be the first to comment