In the UK, the NHS continues to feel the pressure of Chronic Obstructive Pulmonary Disease: COPD exacerbations account for one in eight hospital admissions, and 1.4 million GP appointments annually
CREDIT: This is an edited version of an article that originally appeared in KLTV Online
Chronic Obstructive Pulmonary Disease (COPD) is a growing healthcare challenge – both for patients and for primary care teams. According to the World Health Organisation, COPD was the fourth leading cause of death globally in 2021, responsible for 3.5 million deaths, or 5% of all global fatalities.
As practice managers, you’re in a vital position to lead community-focused COPD strategies that ease system burden, support self-management and ultimately improve patient outcomes.
What Is COPD?
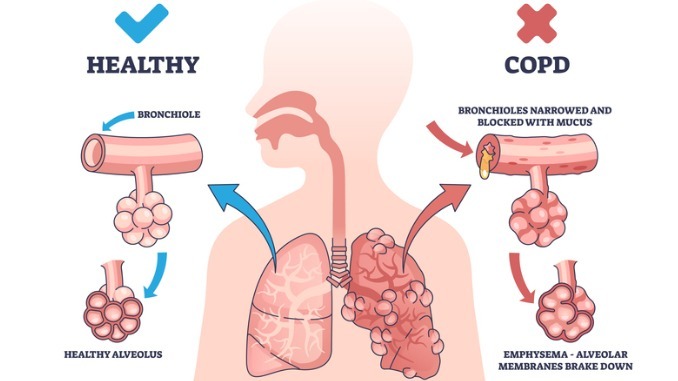
COPD is an umbrella term for progressive lung conditions that restrict airflow and make breathing increasingly difficult. It typically affects people over 50, but symptoms can develop earlier – often going unnoticed until the condition is advanced.
Conditions under the COPD umbrella include:
- Emphysema – damage to the air sacs, reducing the surface area for gas exchange
- Chronic Bronchitis – long-term inflammation of the airways
- Chronic Asthma – in its most severe and persistent form, this can overlap with COPD
The causes of COPD are primarily environmental and lifestyle-related, with smoking being the most common factor. Long-term exposure to air pollution or harmful fumes can also contribute, as can genetic conditions, which make the lungs more vulnerable to damage. These risk factors underscore the importance of early identification and preventive care.
The Practice Manager Role
Early intervention at the community level is critical. Practice managers can play a key role in helping clinical teams identify at-risk patients through routine assessments and the use of tools such as spirometry. Patients presenting with frequent chest infections, shortness of breath, or a persistent cough should be considered for further evaluation, especially if they are over 35 and have a history of smoking or occupational exposure to dust and chemicals.
Supporting self-management is a cornerstone of effective COPD care. Patients benefit significantly from structured education on their condition, including how to use inhalers correctly, how to recognise signs of an exacerbation and how to avoid known triggers. Promoting smoking cessation remains one of the most impactful interventions. Encouraging physical activity can also greatly improve quality of life and reduce hospital visits.
Community partnerships are another powerful tool – by working with local health and wellbeing services, practices can create social prescribing pathways that connect patients to broader support networks. Education is essential, not just for patients but for staff as well. Ensuring that all team members understand how to identify COPD symptoms and know the appropriate referral pathways can make a significant difference. Visible awareness campaigns within the practice – posters, leaflets and digital screens – can help raise patient awareness and prompt early discussions about symptoms.
Creating a Proactive Culture
Ultimately, while COPD cannot be cured, it can be managed effectively. With consistent, proactive community care and a strong emphasis on education and prevention, practice managers can lead the way in supporting patients to live fuller, more independent lives. These efforts not only enhance patient wellbeing but also contribute to more sustainable, responsive primary care services.


Be the first to comment